Let’s Talk Prolapse - Part 2 - Symptoms, Causes and Aggravating Factors
Having a prolapse doesn’t need to feel like a devastating diagnosis. Your vagina is dynamic. It is not static and rigid. It moves and responds to increases and decreases in intra-abdominal pressure through the day as is affected by your activity levels, the amount of time you spend on your feet (versus lying down) and the tasks you are performing. So, in any one day, your prolapse symptoms can vary from hour to hour, depending on these factors.
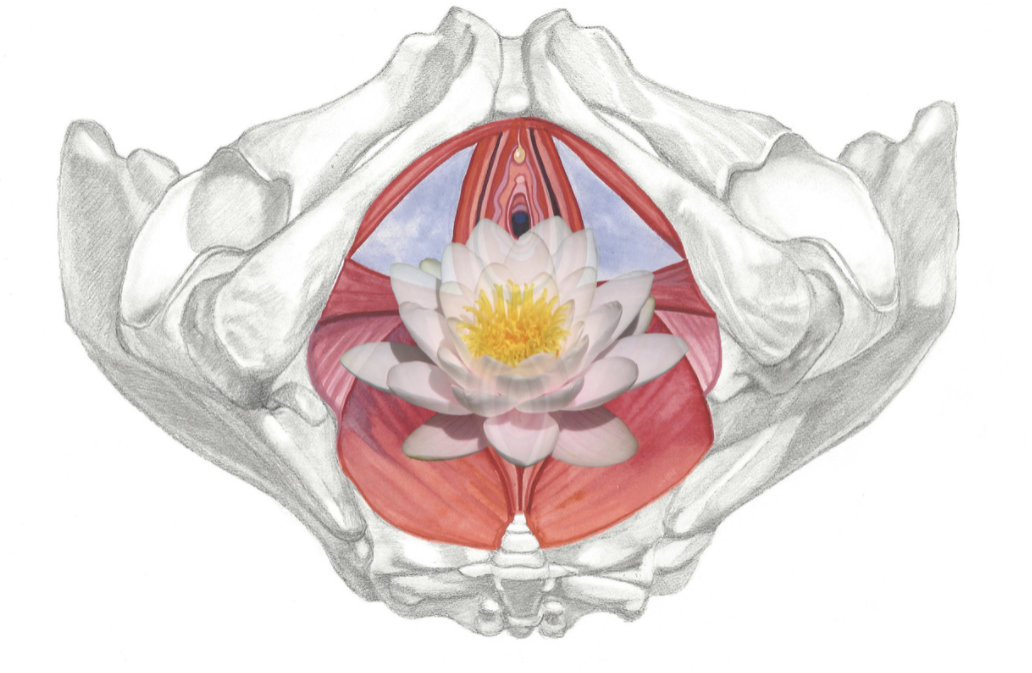
The Symptoms of pelvic Organ Prolapse (POP)
Do you feel any symptoms from your POP? Heaviness, fullness, dragging, bulging, pain? Symptoms depend somewhat on which organ is in descent. As a refresher from last week’s blog, the types of prolapse you may experience are:
Anterior vaginal wall prolapse: prolapsed bladder. You may have some bladder leakage.
Uterine prolapse: prolapsed uterus. You may have backache and discomfort with intercourse.
Posterior vaginal wall prolapse: prolapsed bowel. You may experience constipation and uncomfortable intercourse.
Small bowel prolapse (also known as an enterocele): prolapse of the small intestines. The small bowel descends into the lower pelvic cavity and bulges into the top part of the vagina. You may have a pulling sensation in your pelvis or low back pain, which eases when you lie down.
But wait… hold up… public service announcement:
The severity of your prolapse does not actually correlate to your symptoms at all! Women with the mildest of prolapses may have the severest of symptoms, and women with a physically severe prolapse may have little to no symptoms at all. This is certainly something we see in the clinic all the time and there is so much variability. You might have a mild prolapse and be asymptomatic (have no symptoms), and be living without even knowing it is present. Or you may feel really uncomfortable and have symptoms such as vaginal heaviness or discomfort during sex.
List of possible symptoms:
Vaginal heaviness, pressure or a ‘dragging’ sensation, generally worse towards the end of the day or after a lot of standing/ carrying your baby/ walking.
Intermittent stream when doing a wee
Bladder leakage
Vaginal lump or bulge
Incomplete emptying of the bladder or the bowel when going to the toilet
Feeling like something is “falling out” of your vagina
Unable to keep a tampon in place or feeling like it is lodged incorrectly
Constipation
Low back ache
Vaginal laxity or looseness
Discomfort during sex
Needing to use a finger to splint near or in the vagina when emptying bowels
In severe cases, the vaginal wall or cervix may protrude outside the vaginal entrance.
Diagnosis:
A prolapse is diagnosed by a medical history check and an internal pelvic floor assessment with a Women’s Health/Pelvic Floor Physiotherapist or gynaecologist at your 6-week postnatal check. The internal exam determines the type of your prolapse, the severity of your prolapse, and the function of your pelvic floor muscles. If you didn’t attend this appointment, or you didn’t even know it was recommended, it’s never too late to have a consultation and start taking steps to improve your symptoms and quality of life, even if it is five years down the track.
Common causes/ risk factors of prolapse:
Pregnancy and childbirth (the most common)
Instrumental delivery such as forceps
Carrying and birthing a large baby >4500g
Prolonged second stage of labour (pushing >2 hours)
Multiple births
Returning to high impact exercise too quickly after childbirth
Chronic coughing
Chronic vomiting
Chronic constipation and straining to pass a stool
Obesity
Repetitive manual work and heavy lifting
Gynaecological surgery e.g. Hysterectomy and abdominal surgery
Weak or stretched connective tissue
Weak pelvic floor
Genetic link - if other women in your family have a prolapse
Menopause (leading to low oestrogen levels and weakened tissues)
Get to know your body
There are the different factors that can make your prolapse feel worse. Once you are aware of what aggravates your symptoms, you can work on reducing these, taking steps towards feeling better. Modifying what you do and how you do it is key to reducing your symptoms. It’s not forever, just until your core strength and function improves, your recovery progresses and your symptoms reduce.
Possible Aggravating Factors:
Slacking off with pelvic floor exercises (causing weakness)
Overdoing pelvic floor exercises (causing fatigue and tightness)
Constipation and straining
Change or increase in higher impact exercise including running or lifting heavier weights
Busy days on your feet
Pregnancy
Childbirth
Lifting/carrying your toddler/ child more than usual
A bad cough/ cold/ hayfever
Vomiting
Hormone changes before or during your period
Stress
The good news is that although your prolapse may feel worse at times, it may not actually be worse, as your symptoms don’t always correlate to the severity of your prolapse. As you start to learn what aggravates your symptoms you can take steps to reduce these activities, or take extra rest when you feel your symptoms have increased, to help them settle down again.
Can you treat POP?
Stage 1 and 2 prolapse are very treatable. You can improve your symptoms by seeing a Women’s Health Physio, possibly being fitted for a pessary and following our guidelines.
Stage 3 and 4 are unlikely to resolve with conservative management, however, it is still important to work with your women’s health physiotherapist who can discuss your options and fit you with a pessary. If surgery is required, your women’s health physiotherapist can thoroughly prepare you and your pelvic floor for this.
As a refresher from last week, these are the different stages of POP:
Stage 1: the organ descends to >1cm above hymen (vaginal opening).
Stage 2: the organ descends to just above or below the hymen (within 1cm)
Stage 3: the organ descends >1cm below the hymen
Stage 4: the organ descends completely out of the vagina
We know how all-consuming it can feel to have a prolapse, but please keep in mind that most women get symptom free and back to the activities they love. And this can be achieved without the prolapse being completely resolved! We will dive right into our prolapse management strategies in next week’s blog.