Let’s Talk Prolapse - Part 3 - How can you prevent & treat it?
Our focus in this blog is prevention and treatment of prolapse during pregnancy and postnatally, although many of these strategies are effective at all times. As with so many things in life, the road to recovery is different for every woman, and depends on the stage of your prolapse, the strength and tone of your pelvic floor muscles, your diligence in restrengthening these muscles, your ability to modify your lifestyle, your connective tissue and your genetics. Your recovery will also be slower in the postpartum period, especially if you are breastfeeding, due to hormonal changes you are still experiencing.
You will often notice some improvement soon after implementing the following strategies, but significant results may take several months, so try to focus on the positive change you see, rather than the symptoms you are still experiencing.
It is almost always a good idea to attempt conservative treatment (physiotherapy or pessary) first, as surgery has a considerable failure rate and re-operation rate. If your prolapse is severe, and you do require surgery, you will still need to work on your pelvic floor function prior to and following the surgery, with the guidance of a women’s health physiotherapist.
Read on for strategies to improve and prevent prolapse!
Do your pelvic floor exercises
Regular pelvic floor exercises are the gold standard when it comes to management of pelvic organ prolapse. They have been shown to:
Help prevent prolapse by maintaining a strong support for the pelvic organs.
Treat prolapse by improving the strength of the pelvic floor muscles and therefore the position of the prolapse.
Doing pelvic floor exercises diligently during your pregnancy and again from Day 1 postpartum (whether you birthed vaginally or via caesarean), can help to prevent prolapse. Early activation of your pelvic floor after bub is born helps to re-activate neural pathways to these muscles, helping them to regain strength and motor control. We recommend doing 4-5 gentle pelvic floor contractions each time you feed your baby. Be gentle and don’t cause pain.
To ensure you are doing your pelvic floor exercises correctly (yes many women do them wrong!) so that you gain the rewards of your efforts. Your Women’s Health/Pelvic Floor Physiotherapist will teach you how to engage these muscles correctly, and they will create an individualised exercise plan to help you rebuild your strength.
Want to know more about your pelvic floor? Watch our video with Natalie to learn it all.
2. Avoid constipation and straining
Constipation and straining are the absolute enemy of pelvic organ prolapse. Constipation and straining on their own can lead to prolapse. You need to avoid pushing when you are both peeing and pooping. Make sure you are getting plenty of fluids and enough fibre, as well as talking with your pharmacist about using a stool softener as needed. Your women’s health physiotherapist can also help you with this.
Read last week’s blog: Symptoms, Causes and Aggravating Factors of a Prolapse for more info on what can lead to a prolapse and how it might feel.
3. Stay strong and exercise safely during pregnancy
There’s no way to know what your birth will be like, and you cannot control what happens on the day, but you can be intentional about caring for yourself during your pregnancy and preparing for childbirth.
Participating in a pregnancy-specific program like ours at Bub & Me Physio can increase your chances of an easier labour and recovery, improve your pelvic floor and core function and reduce your likelihood of incontinence, tearing and prolapse.
Join our Strong Mama prenatal program to be guided through your pregnancy, with weekly tailored exercise classes and information videos. It’s offered online so everyone can do it.
4. (Try to) lift nothing heavier than your baby after childbirth
The first 6-12 weeks are a time for recovery and healing. Try to avoid lifting anything that will make you strain—which includes lifting a child, a vacuum, or grocery bags.
Lifting causes increased intra-abdominal pressure which pushes against your pelvic floor. The rule of thumb is to lift nothing heavier than your baby during this time, but if you have a toddler, this gets tricky! They will want to be lifted and carried as well. Try to have lots of cuddles in bed and on the couch, but if you do have to lift them up, encourage them to step up onto a stool or the couch where possible. This way you are lifting them from waist height rather than from the ground and you limit the increase in intra-abdominal pressure you will experience. Before lifting, always first activate your pelvic floor and stay strong in your legs and glutes.
5. Prioritise rest in the first 6-12 weeks after birth
These early weeks are crucial for your postpartum healing. Prioritise horizontal rest throughout the day to facilitate healing of your pelvic floor, which means lying in bed rather than propped up on the couch, eliminating gravity and allowing these muscles to recover. You can lie down to rest when your baby sleeps, and you can also try feeding your baby while lying on your side.
If you had a traumatic delivery with need for assistance then you will need more rest. But that said, if you had an uncomplicated delivery and you feel good, you still need lots of rest to allow your pelvic floor to heal. While YOU may feel fine, your body has gone through nine months of pregnancy followed by childbirth and you are still experiencing huge hormonal changes which continue to impact the strength of your pelvic floor and your whole body. Resting and allowing your body to recover in these early weeks will set you up for better ability to rebuild in the long run.
You can start walking as soon as you feel ready, but this is not a time to push yourself. Start slowly and increase gradually. Walking is great for your mental health, to boost blood flow and to ease constipation, however, don’t be surprised if you feel tired very quickly. You can’t always prepare for just how tired you’ll be. If you have any vaginal heaviness or leakage, this is a sign you’ve pushed too hard, so reduce how far you walk and make sure you get plenty of horizontal rest (in bed) over the next couple of days. And push the pram rather than carry your baby or have someone else carry bub if possible.
6. Have a Women’s Health Consultation at 6-weeks postpartum
The 6-week post-birth consultation compliments your 6-week medical consultation and will include pelvic floor and abdominal separation assessment, a check for prolapse and bladder and bowel health. You will be taught to do pelvic floor exercises correctly, and you will receive tailored guidance on returning to exercise safely, plus anything else relevant to you.
7. Choose appropriate postnatal exercise
While managing a prolapse it’s important to choose low impact exercises that don’t aggravate your symptoms, including gentle walking, swimming, cycling, Pilates, light strength training and gentle yoga. If any activity or exercise doesn’t feel right or causes an increase in your symptoms, then try to avoid it. These modifications are not forever but important while you strengthen your pelvic floor.
In the early months your focus should be on strengthening your core and re-building your functional strength. As your foundations get stronger and your prolapse symptoms reduce, you can start reintroducing higher intensity/ impact activities. This is a gradual process and is best done under the guidance of a Women’s Health Physio.
Returning to running or impact sports too soon can worsen your prolapse. The research recommends waiting until 4 months postpartum, at the EARLIEST, to start jogging, and even longer for higher intensity training such as running or impact sport, abdominal crunches, full frontal planks, low squats and heavy weights.
The best thing you can gift yourself during this time is access to tailored, postnatal-specific exercise classes and education so you can safely rebuild your core and pelvic floor, improve your prolapse symptoms and restrengthen.
This is what we offer in our Strong Mama Postnatal Program.
8. Get inverse everyday
This means elevating your pelvis above your heart. This position uses gravity to bring your prolapse back into a better position. Try putting 2 pillows under your pelvis to elevate it. You can lie on the floor and prop your feet up on the couch. Hold this position for at least 10 mins, preferably in the afternoon, or when you are feeling symptomatic. As you get stronger you can try going into a bridge position to invert your pelvis.
9. Practice good posture
Slouching on a chair in front of your PC, or hours spent slumped forward feeding and caring for your baby don’t do anything good for your prolapse. Sitting and standing upright with a neutral spine helps to activate your core (pelvic floor and deep abdominal muscles). This in turn helps support your internal organs and provides stability to your pelvis and spine. Think about your sitting posture and your set up. Make sure you have lumbar support, and extra pillows as needed to support you when you’re feeding bub.
10. Exhale with the exertion
When you have increased pressure from lifting weights or impact with running or jumping, holding your breath or bearing down can exacerbate the issue. Make sure you exhale with exerting effort, including pooping, lifting your baby, lifting a laundry basket or pushing a piece of furniture. If you are holding your breath to do a task then it is too hard.
11. Get internal/ external support
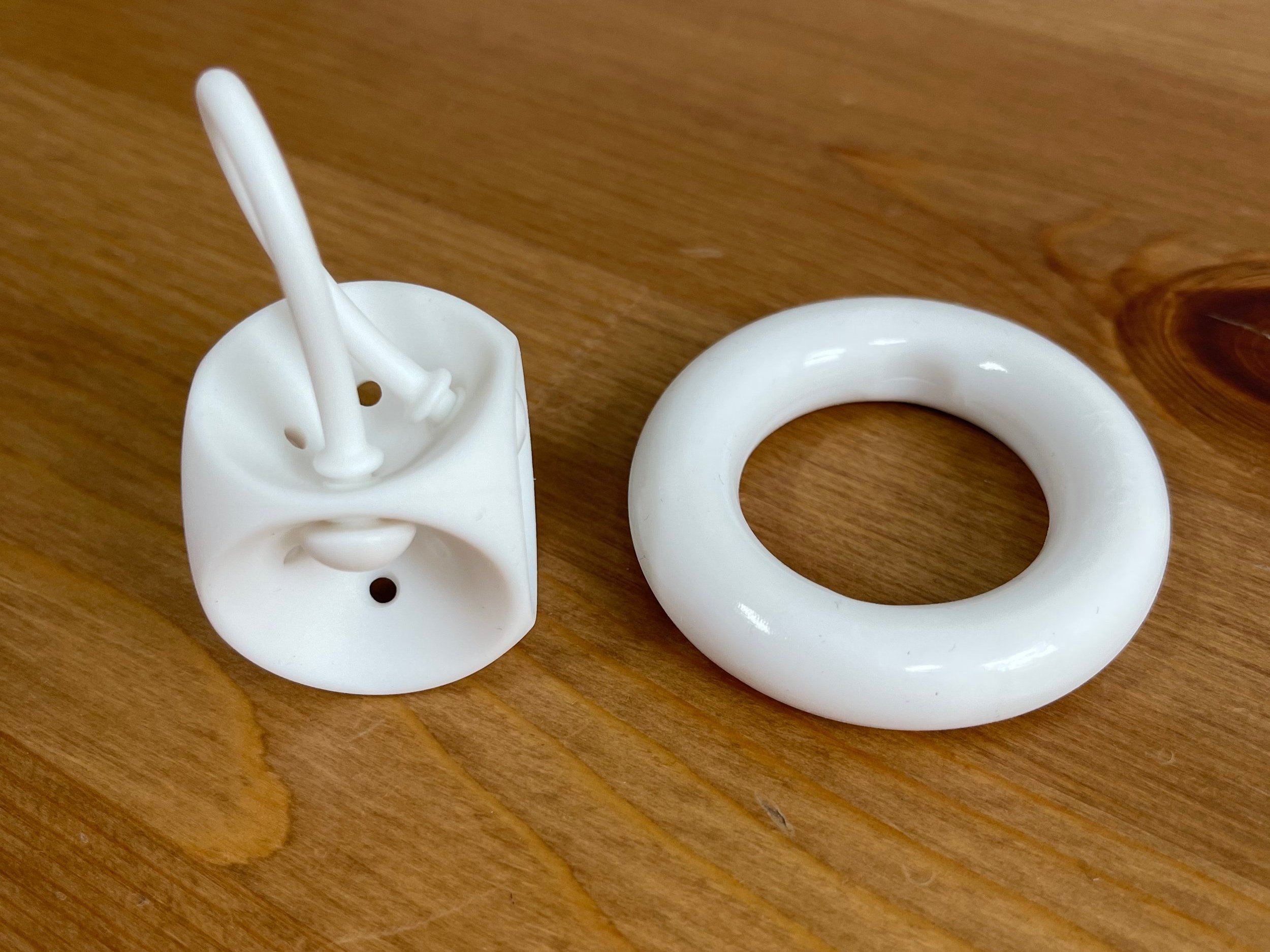
See your women’s health physio and discuss using a compressive garment to provide external support or getting fitted for a pessary.
A pessary is a silicone device inserted into the vagina to support the prolapse and the weakened pelvic tissue. You may wear the pessary all the time, or just when working out to provide internal support to your vaginal walls.
Getting a pessary is OKAY and can help support your pelvic floor while you stay active and work on building your pelvic floor strength.
12. Weight loss (if you are overweight)
Carrying increased weight places increased pressure on your pelvic floor. We know that losing weight can be a challenge, but even losing a couple of kilos can make a positive difference. Going about this on your own can be tough, and we recommend consulting with a Dietician for advice and guidance.
13. Seek treatment if you have a cough or cold
Coughing, sneezing and blowing your nose, places a lot of pressure on your pelvic floor. Activate your pelvic floor before you cough or sneeze and see your Doctor for treatment.
14. Consider using vaginal oestrogen
If you are breastfeeding your oestrogen levels are low, which impacts your vaginal tissue and muscle strength. Oestrogen helps to keep the pelvic floor muscles toned. When you are breastfeeding and have low oestrogen, your pelvic floor muscles and vaginal skin become thinner, weaker and less elastic. Speak to your GP about getting a prescription for vaginal oestrogen, which can help to improve the quality and strength of the vaginal tissue. Also bear in mind that once you stop breastfeeding and your oestrogen increases, your tissue strength will improve and your prolapse symptoms may reduce!
Hopefully this information helps. Please remember, you are not alone. There are a wealth of health professionals who can help!
As always, reach out if you have any questions.
P.S. If you’d like to start reading the prolapse blog series from Part 1, jump across to the first blog here: Let’s Talk Prolapse - Part 1 - What is it?
References:
Braekken IH, Majida M, Engh ME, Bo K (2010) Can pelvic floor muscle training reverse pelvic organ prolapse and reduce prolapse symptoms? An assessor-blinded, randomized, controlled trial. American Journal of Obstetrics and Gynecology 203: 170-177.
Dietz, HP (2015) Pelvic organ prolapse – a review. Volume 44, Issue 7, July 2015
Dietz HP (2008) The aetiology of prolapse. Int Urogynecol J,19:1323–29.
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2013) Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. Br J Obstet Gynaecol;120:152–60.
Hagen S, Stark D (2011) Conservative prevention and management of pelvic organ prolapse in women (review). Cochrane Database of Systematic Reviews: 1-72.
Rogers and Fashokun (2016) Pelvic organ prolapse in women: epidemiology, risk factors, clinical manifestations, and management. 1-11.
Thompson, JA, O'Sullivan, PB, Briffa, KM, Neumann, P (2006) Assessment of voluntary pelvic floor muscle contraction in continent and incontinent women using transperineal ultrasound, manual muscle testing and vaginal squeeze pressure measurements. Int Urogynecol J Pelvic Floor Dysfunction. 17(6):624-30.
Whiteside JL, Weber AM, Meyn L, Walters MD (2004) Risk factors for prolapse recurrence after vaginal repair. American Journal of Obstetrics and Gynecology. 191: 1533–1538.